FAQ: Hip Impingement (FAI – Femoroacetabular impingement)
06/05/24What is hip impingement? Hip impingement, also known as femoroacetabular impingement, happens when extra bone grows inside the hip joint over time. This growth can limit hip movement and potentially harm the cartilage.
What are some symptoms of hip impingement? People often feel sudden pain after certain movements like squatting or repetitive activities like running. The pain is typically felt at the front of the hip and can also be in the groin, back, or sides of the hip.
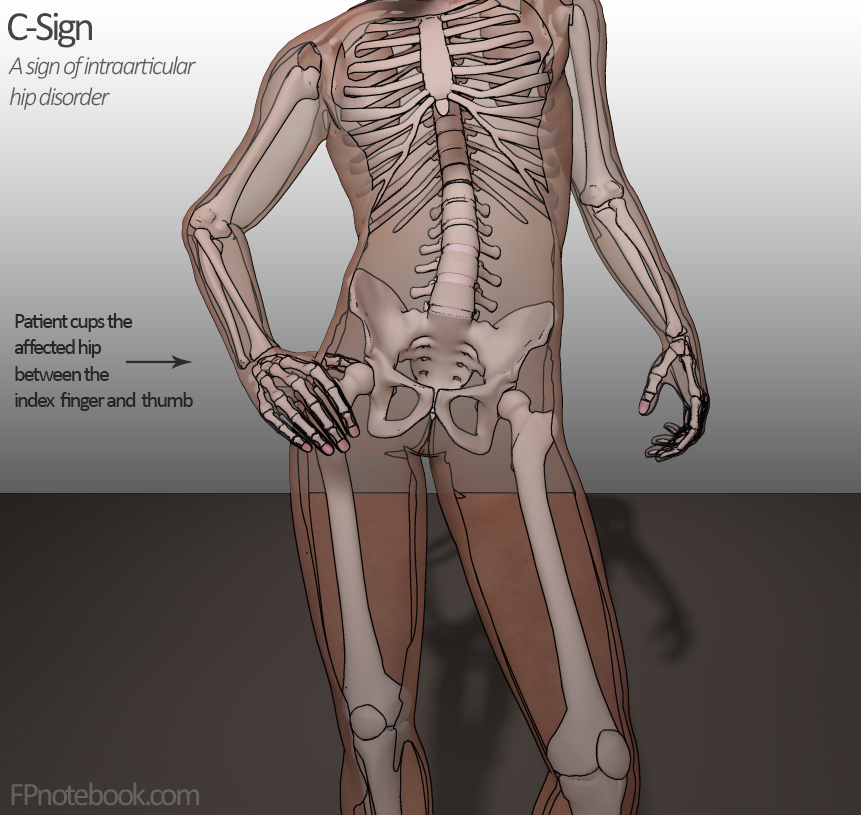
Where will I feel pain? Pain is usually around the hip joint, with common spots being the front of the hip. Sometimes, it can feel like a “C” shape around the hip when touched.
What activities or movements trigger pain? Deep bending of the hip (like squatting) and crossing legs can be painful. Sitting in uncomfortable positions might also cause achy feelings if the cartilage is affected.
What causes hip impingement? Hip bones respond to stress by growing more bone. This can limit movement and cause pain, especially in people genetically prone to this condition.
What are the initial steps for relief? Seeing an osteopath or physiotherapist for a thorough examination and treatment is highly recommended. They can provide symptomatic relief with manual therapy. Using foam rollers or trigger balls to release tight muscles around the hip and lower back can help ease symptoms initially and can be performed by yourself. Trigger ball release to the glute muscles & foam rolling the quadriceps and adductor muscle groups can help.
What things to avoid? Avoid deep squatting and leg crossing to prevent worsening symptoms in the short term.
What are some rehabilitation exercises? Strengthening hip and core muscles is crucial. A 12-week program of exercises can improve function and reduce symptoms. It’s important to assess and strengthen muscles that support the hip joint. Your health professional may promote strength development in the gluteal region as a start.
What is the expected rehabilitation time? A minimum of 12 weeks is expected for rehabilitation, depending on the severity and adherence to the rehabilitation program.